Last updated on December 10th, 2025

In applied behavior analysis (ABA) therapy, your session notes don’t just reflect what happened during a therapy session—they determine whether you get reimbursed, how well you track client progress, and if your clinic stays compliant. Good ABA session notes are a critical component of effective care and a powerful tool for behavior analysts and ABA providers alike.
But here’s the truth: writing effective ABA session notes that meet insurance requirements, support client outcomes, and fit into your workflow is no small feat. Between managing therapy sessions, collecting data, and ensuring medical necessity, note-taking often becomes a burden—especially for small clinics juggling client care and administrative demands without dedicated support.
That’s why we’re here. Whether you’re a BCBA, RBT, or clinic administrator, this guide breaks down how to write good session notes for insurance, step-by-step. Along the way, we’ll show how technology—like Raven Health’s all-in-one practice management software—can turn session notes from a compliance headache into an AI-powered advantage.
At the heart of behavior analysis is the ability to capture and analyze what actually happens during a session. Your notes are more than documentation—they’re a record of how each component of ABA is delivered in real-time. Whether you’re reinforcing functional communication skills, running a discrete trial, or managing challenging behavior, detailed and comprehensive notes help tell the full story of the session and make it easier to justify the necessity of the services provided.
For individuals with autism spectrum disorder and other developmental disabilities, consistent progress tracking is essential. High-quality session notes provide valuable data that supports clinical decision-making, highlights trends, and helps teams adapt programming as needs evolve. Without clear and accurate notes, it’s nearly impossible to demonstrate the effectiveness of your interventions or secure continued insurance coverage.
Timeliness matters, too. Session notes should be completed immediately after the session—while the details are still fresh. Waiting too long can lead to missed insights or gaps in documentation, both of which can affect reimbursement and care quality. With the right tools in place, you can streamline the process so your notes remain accurate, thorough, and aligned with best practices in ABA documentation.
What Are ABA Session Notes?
ABA session notes are detailed documentation of what occurred during an ABA therapy session. These notes serve as a legal and clinical record and play a pivotal role in tracking progress, highlighting the need for ongoing therapy, and supporting billing claims with insurance providers.
The right session notes go beyond just logging time. They offer clear and concise language describing the client’s behavior, targeted strategies used (e.g., functional communication training, discrete trial training), and the client responses observed. These records should accurately reflect observable behaviors and relevant environmental factors, offering objective data that informs future interventions.
Effective ABA session notes ensure that therapy is not only clinically sound—but also insurance-compliant.
Elements of an ABA Session Note
Effective session notes typically include the following components:
- Client Information: Name, date of birth, session date, and therapist name
- Session Summary: Brief overview of the therapy session and goals targeted
- Behavioral Objectives: Target behavior(s) addressed and skill acquisition plans used
- Specific Interventions: Description of ABA strategies implemented (e.g., picture exchange communication system, DTT)
- Client Responses: Objective descriptions of how the client responded
- Behaviors Observed: Clearly stated, observable behaviors including frequency, intensity, or duration
- Relevant Environmental Factors: Any variables that may have impacted behavior
- Progress Toward Goals: Tracking of how the client is moving toward mastery
- Parent or Caregiver Involvement: Notation of any caregiver training or feedback
- Signature: Legible full legal signature of the session provider
- Timestamp: Start and end time of the session
These detailed session notes are more than a formality—they’re a comprehensive record of your client’s care and a key part of the ongoing process in ABA therapy.
Why Insurance Compliance is Important
Insurance companies demand accurate documentation to approve and reimburse claims. If your ABA session notes don’t show clear justification for treatment, track patient progress, or follow a structured framework, your claims can be delayed or denied.
Good ABA session notes play a critical role in insurance compliance. They must:
- Objectively describe session details
- Demonstrate progress toward treatment goals
- Provide supporting data collection
- Include clinical techniques and behaviors observed
- Align with your treatment plan
In short, insurance providers rely on your notes to make informed decisions—and so should you.
Clear and consistent note-taking isn’t just for compliance—it’s central to quality behavior analysis. Every session note should help communicate how treatment aligns with your clinical rationale and supports meaningful gains for the individual.
If you’re unsure where to begin, reviewing ABA session note examples can offer helpful insight. Seeing how effective notes are structured gives your team a stronger foundation to build from—and helps standardize documentation across providers.
When notes are done well, they don’t just check boxes; they help track real patient progress. You’ll be able to identify trends, adjust interventions, and confidently communicate outcomes to caregivers and payers alike.
Remember: the goal of ABA therapy is meaningful, measurable change. Writing effective notes ensures every session contributes to that change, one data point at a time.
For a deeper dive into staying compliant, check out our guide to ABA compliance.
Best Practices for Writing ABA Notes
Be Objective and Behavior-Focused
Effective ABA session notes must be based on objective data, not subjective language. Instead of writing “the client seemed upset,” say “the client cried and threw objects for 3 minutes following the transition cue.”
This shift from subjective impressions to observable behaviors provides clarity—and is essential when demonstrating medical necessity to insurance companies. Behavioral analysis thrives on measurable action, not assumptions.
Use objective descriptions to reflect:
- Specific behaviors
- Client responses
- Observable interactions with therapists or caregivers
- Environmental influences

Use Consistent Terminology and Format
Whether you’re writing RBT session notes or BCBA documentation, consistency is key when it comes to tracking client progress. Insurance companies expect standardized formatting that aligns with formal and clinical language, in addition to an established clinical language in applied behavior analysis.
That’s why many clinics now rely on practice management software like Raven Health to auto-generate session note templates with built-in compliance formatting. These tools support legibility, reduce errors, and streamline documentation so your notes immediately meet payer expectations.
Document Progress Toward Goals
Session notes should clearly demonstrate progress—or lack of it—toward identified goals. This is where data collection comes in. Good ABA session note-taking combines a narrative with data to show:
- How the client performed on specific targets
- What adjustments were made based on the client’s progress
- Trends observed across multiple sessions
Tracking progress over time helps identify patterns, supports future sessions, and justifies the continuation of services.

ABA Session Notes Examples
Looking for ABA session note examples that strike the right balance between detail and clarity? Here’s a sample breakdown of what kind of context ABA session notes contain:
Sample ABA Session Note
| Section | Example |
|---|---|
| Client Info | Name: Jane Doe, DOB: 03/22/2019, Session Date: 5/10/2025 |
| Session Summary | A 2-hour session focusing on communication skills and reduction of aggressive behavior. |
| Interventions Used | Picture exchange communication system (PECS), discrete trial training (DTT), and functional communication training (FCT). |
| Behaviors Observed | Threw objects (3x), screamed (2x), requested break using PECS. |
| Client Progress | The client successfully completed 8/10 trials of requesting using PECS, an increase from the previous session (5/10). |
| Signature | RBT Jane Smith, 5/10/2025 |
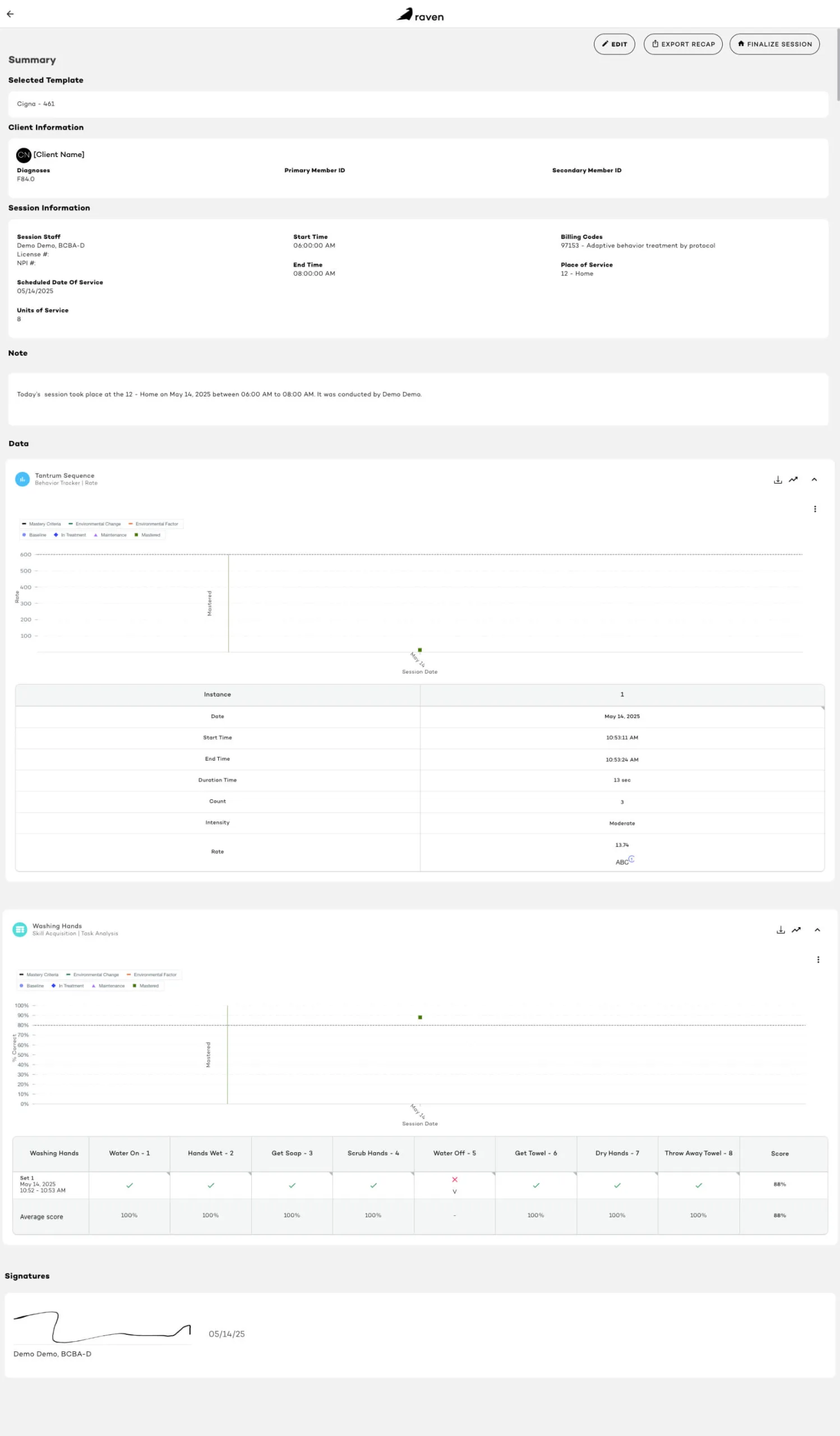
For a view of Raven’s simplicity, check out a screenshot of a sample session note below:
| Feature | RBT Notes | BCBA Notes |
|---|---|---|
| Focus | Implementation details, client behavior, session details | Treatment planning, supervision notes, goal review |
| Data Collection | Trial-by-trial data, evidence-based methods | Analyzing data trends, modifying goals |
| Documentation Depth | Focused on session-specific observations | Higher-level interpretation and planning |
| Signature | RBT full legal signature | BCBA full legal signature and credentials |
RBT vs. BCBA Note Differences
Both sets of notes serve the same function: to create an accurate and comprehensive record of the client’s care, while tracking specific behaviors and achievements.
How to Choose the Best ABA Session Note Format
The format of your ABA session notes should align with your role:
- RBTs may prefer structured templates with checkboxes and dropdowns for quick, accurate documentation of specific behaviors.
- BCBAs need space to write comprehensive notes and analyze data trends, requiring flexibility and customization.
- Behavior Analysts or Clinical Supervisors may rely on software-generated summaries to oversee treatment fidelity and progress.
- Administrators should look for a format that supports billing, compliance, and audit-readiness.
Raven Health’s AI-powered platform adapts documentation to your role—streamlining the note-taking process without sacrificing accuracy or detail.
Tips for Writing Session Notes for Insurance
Writing ABA session notes for insurance can feel overwhelming, but these actionable tips can help:
- Write notes immediately after the session to ensure accuracy
- Use clear and concise language—avoid jargon or vague terms
- Describe observable behaviors (e.g., “client hit peer 3 times”)
- Avoid subjective language like “appeared sad” or “seemed happy”
- Link behaviors to specific interventions (e.g., “FCT used to reduce aggression”)
- Track progress from the previous session for continuity
- Use a professional tone and structured format
- Ensure accurate documentation of all session details
- Include a legible full legal signature
- Double-check for completeness before submission
Documentation isn’t just about compliance—it’s a valuable tool to identify trends and support informed decisions about future interventions.
In applied behavior analysis, session notes are a reflection of both the clinical and administrative sides of your practice. Whether you’re recording a target behavior, noting a specific intervention, or logging a client’s date of birth, these notes serve as a record of care and a roadmap for treatment planning.
Session notes should always highlight components of ABA in action—reinforcement strategies, prompting procedures, and data collection that align with each client’s goals. Well-crafted RBT session notes, for example, can provide behavior analysts with insight into what’s working (or not) between supervision visits.
Consistency in note taking leads to consistency in care. When session notes are written clearly and updated regularly, they support measurable client progress and help behavior analysts make timely, data-driven decisions.
Ultimately, high-quality session notes are foundational to behavior analysis. They connect everyday actions to broader outcomes and ensure that every service delivered in ABA therapy is traceable, accountable, and impactful.

The Final Word: Power Up Your ABA Practice With Better Notes
Writing effective ABA session notes isn’t just a requirement—it’s an opportunity.
The note-taking process improves client outcomes, demonstrates the need for clinical services, reduces denials, and fuels your clinic’s growth. And when done right, session notes play a starring role in everything from insurance claims to long-term client progress.
But if you’re still relying on manual note-taking, you’re leaving revenue—and time—on the table. That’s where Raven Health comes in.
Our AI-powered, all-in-one practice management software takes the pressure off your providers by automating ABA session notes, data collection, billing, and compliance tracking. It’s designed for the exact needs of small to mid-sized ABA therapy clinics—no more toggling between disconnected systems or scrambling for last-minute documentation.
Want to streamline your operations and strengthen your ABA practice? Raven offers free a free demo overviews if you’re simply interested in learning more.
Whether you’re ready to launch or scale, Raven Health helps you start an ABA company built for efficiency, compliance, and impact.
And don’t forget to explore the latest trends reshaping the ABA industry in 2025—because the future is AI-powered, and your practice deserves the edge.