ABA Compliance: What You Need to Know
What is ABA Compliance?
ABA compliance involves strict adherence to regulatory standards and the implementation of uniform federal accessibility standards, as mandated by various federal laws. Clinics often seek ABA professional certifications to validate their practices; for example, many providers have earned ABA professional certifications to further demonstrate compliance with state regulations and relevant laws. Ensuring that each site properly provides secure data storage, integrates modern software solutions, reflects newly constructed design trends, and accommodates both staff and client needs is paramount.
Personnel in the clinic must be responsible for maintaining compliance at every level to ensure a consistent approach to meeting regulatory standards. In accordance with the Disabilities Act, organizations must follow, observe, and update practices as outlined by this law, ensuring full respect for its provisions. While compliance with regulations such as the Disabilities Act is mandatory, in certain cases, specific waivers may apply. These waivers allow exemptions from particular provisions of the law under strict guidelines, offering flexibility for certain operational adjustments. Regular education and training help determine staff knowledge and adherence to laws, ensuring that the team is equipped to manage site tasks effectively and stay up-to-date with regulatory standards.
Ongoing audits are a critical aspect of maintaining adherence to federal and state regulations. ABA providers must be subject to regular audits to ensure that all operations, from data collection to billing, consistently meet required standards. This helps in identifying any gaps in compliance before they become significant issues. Periodic changes to protocols, including scheduling and record-keeping, help maintain compliance with these laws and further advocate adherence.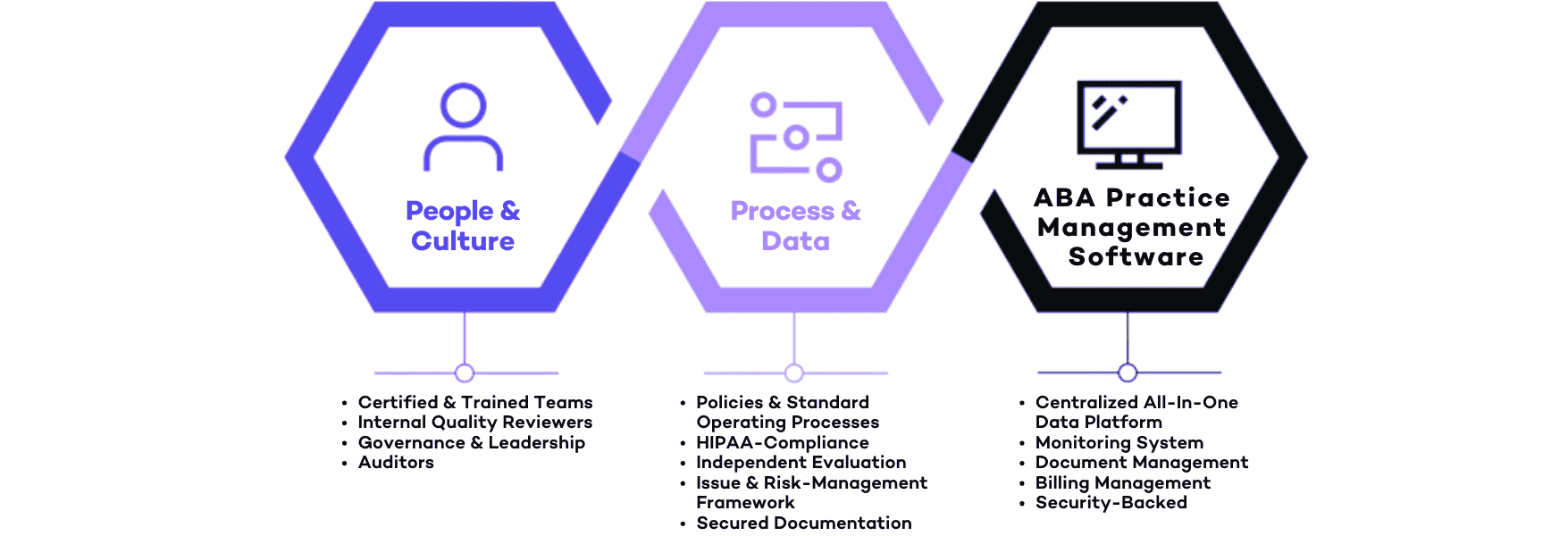
Regulations and Standards for ABA Practices
ABA therapy operates under strict guidelines designed to protect client information and financial integrity. Many practitioners enhance their qualifications through education by obtaining up-to-date ABA certifications. In fact, several renowned facilities require ABA professional certifications as part of their recruitment process. Personnel who are responsible for implementing practices often pursue additional ABA professional certifications, ensuring their expertise is recognized and practices adhere to the most current standards.
Maintaining HIPAA Standards in ABA Therapy
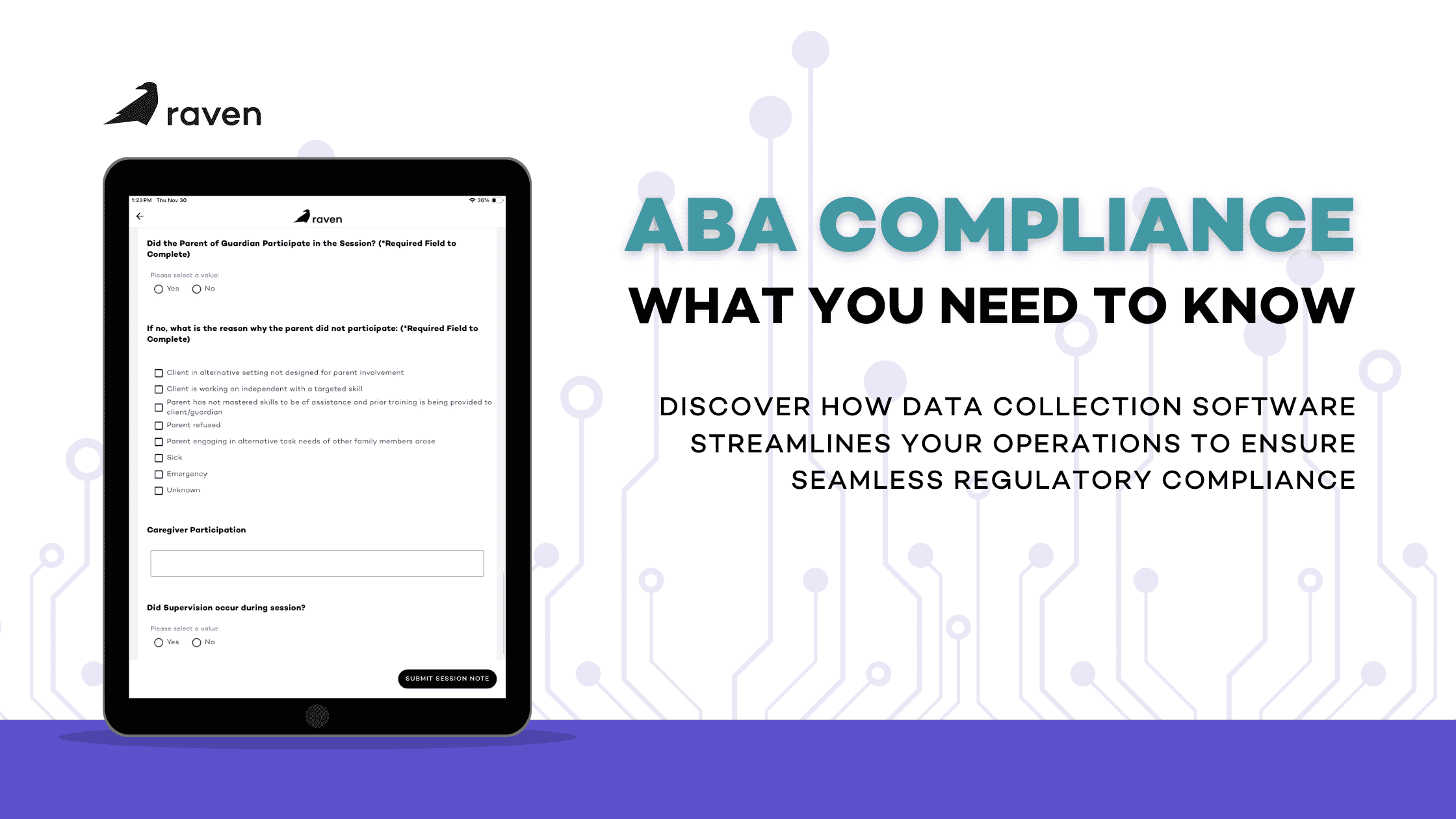
The Health Insurance Portability and Accountability Act (HIPAA) is essential for compliance in ABA practice management, especially regarding the site’s security of patient data. ABA professional certifications ensure that practitioners are properly trained to manage confidential information. Data collection systems must be HIPAA-compliant, with robust encryption and secure storage protocols. Compliance with HIPAA standards means that facilities can securely manage appointments and maintain client confidentiality.
Facilities and Structural Compliance
Facilities must be designed to meet the highest structural and operational compliance standards, including adherence to the Architectural Barriers Act for barrier-free access. This includes ensuring that water closets meet accessibility guidelines, providing ease of use for all individuals. Regular updates ensure these facilities stay aligned with newly-dated state and federal regulations. Equipped with advanced technology for security and privacy, these facilities undergo frequent reviews to ensure ongoing compliance and maintain optimal patient care. The continuous integration of new compliance measures reinforces our commitment to maintaining modern, safe, and fully compliant environments.
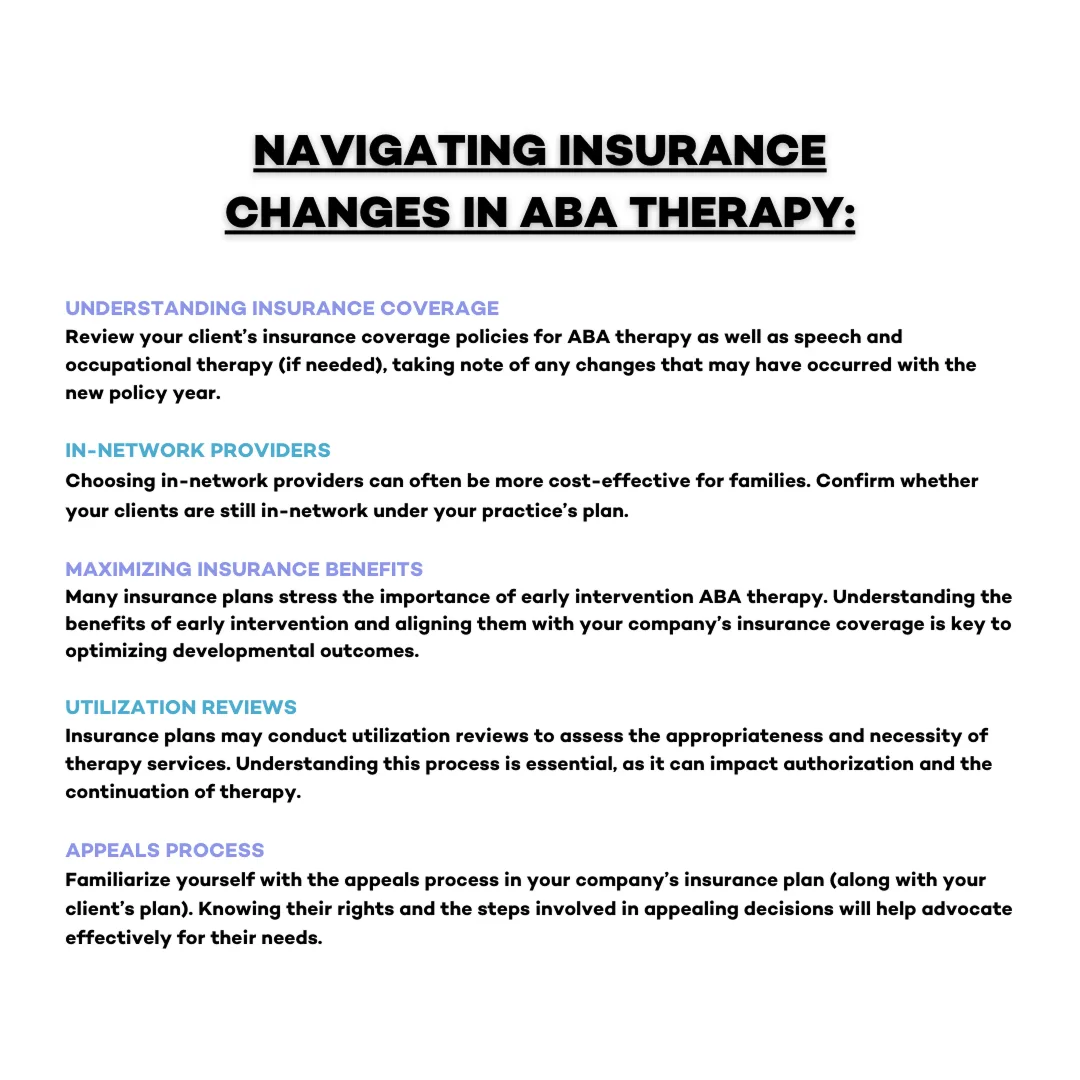
Insurance and Billing Regulations
Accurate billing and insurance claims processing are integral to ABA clinical operation, governed by both state laws and federal regulations. ABA billing software must ensure compliance with payer requirements, reducing denials and improving revenue cycle management. Billing services should aim on accuracy, utilizing automated processes to avoid errors. This is part of the process of confirming that all billing codes and documentation are in line with current laws and regulations. To learn more about optimizing ABA billing, check out our guide on ABA Billing.
Tools and Resources for Regulatory Compliance
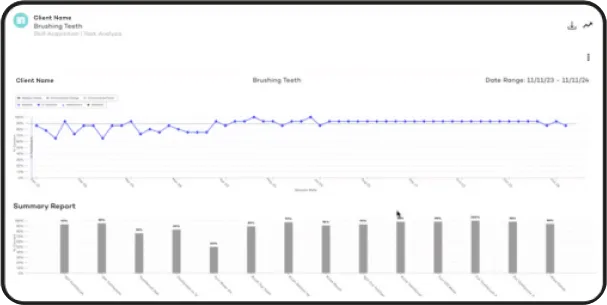
Implementing the right software can significantly improve compliance and operational efficiency in ABA therapy practices. All-in-one ABA platforms offer automated features for billing, scheduling, and regulatory auditing, which helps reduce the administrative burden and ensures compliance with both federal and state regulations. Integrated scheduling and billing systems facilitate practices in delivering timely care while maintaining compliance. Software verification plays a crucial role in ensuring process accuracy and regulatory adherence. With robust solutions, ABA practices can streamline site workflows, ensuring that all patient interactions are properly documented and fully compliant. These tools also help ensure facilities are covered under the appropriate regulations and maintain authority over their operations.
ABA Compliance Software Solutions
A well-structured ABA practice requires both data collection software and reliable management systems to streamline operations. These systems help providers meet standardized federal accessibility regulations, reduce administrative tasks, and focus on client care. Compliance software should assist modifications for accessibility, ensuring that the site properly adheres with the Disabilities Act and Architectural Barriers Act. In addition, verification processes ensure that all procedures are conducted with the expected level of accuracy and compliance.
Automated Billing and Documentation Tools
A well-structured ABA practice requires both data collection software and reliable management systems to streamline operations. These systems help providers meet standardized federal accessibility regulations, reduce administrative tasks, and focus on client care. Compliance software should assist modifications for accessibility, ensuring that the site properly adheres with the Disabilities Act and Architectural Barriers Act. In addition, verification processes ensure that all procedures are conducted with the expected level of accuracy and compliance.
Staff Training Programs and Resources
Regular training programs are essential to ensure that staff members understand regulatory requirements, adhering to HIPAA standards, and following best practices. ABA providers can rely on these programs to equip staff with the skills necessary to manage site tasks effectively while keeping up-to-date with their ABA professional certifications.
Additionally, these programs ensure that any adjustments made to facilities for compliance are aligned with the Disabilities Act. Training also helps staff meet minimum compliance requirements, ensuring that essential legal standards are consistently upheld. Proper verification ensures that staff are well-trained and certified, with the backing of the facility’s department overseeing training initiatives.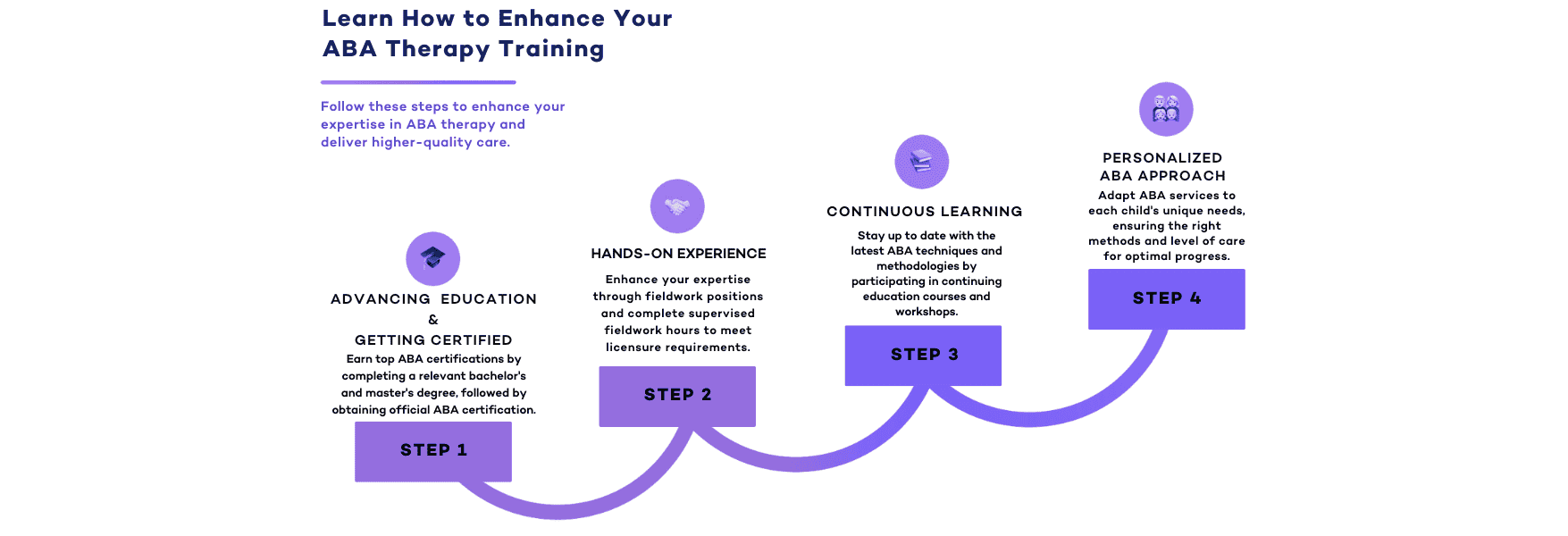
Compliance Checklists and Auditing Tools
Checklists and auditing tools embedded within ABA software help providers track compliance across different aspects of the business, from HIPAA regulations to billing procedures. Verification ensures that any discrepancies are identified and corrected before proceeding with claims or treatments. Using these tools, ABA practices can maintain high standards of documentation and reduce the risk of non-compliance. With the right auditing system, practices can ensure that their site properly operates throughout different departments and remain compliant with federal accessibility standards and state-specific regulations. Regular investigation of audit findings and complaints helps to address any gaps in compliance before they escalate into issues.
HIPAA-Compliant Data Management Systems
Data security is a cornerstone of ABA practice management. Providers must utilize software that meets HIPAA standards and ensures secure data collection, storage, and accessibility. Industry professionals must have a strong education with ABA professional certifications to ensure they are capable of maintaining compliance with these standards. This verification ensures that data is reviewed regularly for compliance coverage, minimizing the risk of breaches. A mobile-friendly platform also provides ABA professionals with access to patient information securely from any site, improving workflow and patient care.
Additional Benefits of ABA Practice Management Software
ABA software not only helps ensure compliance but also provides operational benefits, such as streamlining scheduling, payroll, and accounts receivable oversight. Integrated systems are intended to help improve the efficiency of ABA facilities, allowing providers to deliver services without distraction. By ensuring that the software meets accessibility requirements, providers can deliver services in line with standardized federal accessibility regulations. The integration of design modifications ensures that clients have full access to the resources and support they need. This ensures that the software and systems in use comply with industry regulations.
Grants and Funding for Compliance
ABA providers may also benefit from grants that support compliance initiatives. Many federal agencies provide funding for improving accessibility and meeting the Disabilities Act requirements. Providers may be eligible for federal funds that assist with making necessary modifications to facilities, ensuring that their practice remains compliant with national standards.
By applying for loans or financial aid, practices can strengthen their operations while adhering to regulatory requirements, including considerations of value-based care models. For more details on value-based care versus fee-for-service models, read our post on Value-Based Care vs. Fee-for-Service.
Providers should stay in close connection with their department to learn about accessible funding opportunities that can help with these efforts. Department heads can offer valuable insights and guidance on proceeding with the application process and meeting eligibility requirements. A verification process ensures that applications are completed accurately and submitted on time.
Applying for these grants allows ABA providers to make necessary modifications to facilities while ensuring that their practice remains compliant with national standards. This funding can also help aid other facilities covered under state and federal accessibility guidelines.
Many federal agencies, including the General Services Administration (GSA), provide funding for new construction and facility upgrades to enhance accessibility and ensure compliance with the Disabilities Act and the Rehabilitation Act. Providers may be eligible for federal grants to aid the necessary changes, ensuring their practice meets national accessible standards
However, construction tends to come with a hefty price-tag. With that said, federal government agencies may have limited funding opportunities available, so it’s important to apply early and provide the necessary documentation to maximize eligibility. Providers seeking financial requests (including loans) for construction projects should also be prepared to submit documentation on behalf of their organization, demonstrating the need for accessibility improvements.
Ray ID & Site Management
ABA practices need to integrate digital tools that aid in site security and performance. Ray ID is a key tool for tracking errors and improving performance metrics. By using Ray ID, ABA providers can monitor site operations and ensure compliance with accessibility and security standards. When issues arise, Ray ID helps identify errors related to data transfer or communication, allowing for quick troubleshooting.
By leveraging Ray ID, ABA practices can track ongoing performance metrics, identify security vulnerabilities, and address any compliance gaps before they become significant issues. This makes Ray ID a crucial tool in maintaining a reliable and compliant online presence for ABA providers.
Conclusion
ABA practice management requires careful attention to compliance with various healthcare regulations, including HIPAA, insurance, and state-specific laws. By implementing an effective all-in-one software solution, ABA professionals can streamline their operations, enhance client care, and maintain financial security. ABA practices must concentrate on site accessibility, ensuring that their facilities comply with regulatory requirements. This is an essential step in the process of maintaining compliance. By addressing compliance requests proactively and maintaining a structured response system for complaints, ABA providers can prevent regulatory violations and enhance service quality. By adhering to these standards, ABA providers ensure that they are delivering the highest level of care while optimizing their operations.
Raven Health offers a free 30-day trial to help your ABA clinic stay on track effortlessly. Sign up today and experience the benefits of automation and efficiency with the industry’s best practice management software.