The Best ABA Note Templates: Real ABA Session Note Examples & Documentation Tips
When you’re an Applied Behavior Analysis (ABA) therapy provider, your mission is clear: deliver exceptional care. But complex billing processes, insurance requirements, and claim denials can get in the way of that goal — draining time, cash flow, and energy from your ABA therapy center.
When it comes to applied behavior analysis (ABA), few tools are more vital than a well-structured ABA session note template. Whether you’re a registered behavior technician (RBT), a board-certified behavior analyst (BCBA), or an ABA practice owner, mastering your ABA session notes can truly transform your daily work — saving time, improving accuracy, and ensuring every therapy session counts toward meaningful change.
At its core, great ABA session notes aren’t just paperwork — they’re the foundation of your entire documentation process. When done right, they become a living record that helps ABA therapists and supervisors align on goals, share updates with parents and healthcare providers, and demonstrate that your clients are making real, measurable strides.
Strong, effective session notes help your team track progress in a clear, consistent way. Each note captures the small, incremental victories that add up to big gains over time — from increasing desirable behaviors to minimizing barriers that hold clients back. Without detailed, organized session notes, it’s nearly impossible to make data-driven decisions or plan smart, targeted future interventions.
Equally important, well-crafted notes protect your practice by proving that every claim you submit is backed by solid, measurable data. Insurance companies and auditors want to see that you’re delivering high-quality services and meeting the requirements that keep funding flowing. Accurate notes safeguard your clinic from compliance headaches — and help you get paid faster.
Today you’ll find:
- Proven ABA session notes examples you can trust
- A practical notes template you can adapt instantly for your own clients
- Pro tips for faster, clearer note-taking
- A game-changing look at Raven Health’s all-in-one, AI-powered session notes tool — the only solution in the industry that writes your notes for you at no extra cost
Whether you’re logging ABA therapy sessions for young learners with autism spectrum disorder or adults working on daily living skills, you’ll learn how to build effective session notes that help your entire team communicate better, demonstrate real progress to funders, and plan the right future interventions to keep each client growing.
Let’s get started — and help you reclaim hours of admin time in your ABA practice, so you and your team of ABA therapists can stay focused on what you do best: changing lives.

Applied Behavior Analysis ABA: Why Session Notes Matter in Therapy Sessions
Applied behavior analysis (ABA) is the gold standard for evidence-based behavior therapy — especially for people with autism spectrum disorder.
But here’s the thing: your outstanding ABA therapy sessions only count if they’re documented properly. Strong ABA session notes help you:
- Prove client progress to insurance companies
- Plan smart future sessions
- Ensure compliance
- Keep everyone — therapists, parents, other healthcare providers — aligned
Your session notes are more than paperwork. They’re your best tool for better client outcomes. Each note becomes part of a comprehensive record that clearly shows how a client is responding to treatment over time. Effective, detailed session notes also help you address communication issues that can happen when multiple team members work with the same client, making it easier for everyone to stay in sync and support goals consistently.
When your notes serve as clear, factual evidence of a client’s journey, it’s easier to justify services, secure funding, and plan next steps. Effective notes are a critical safety net for your practice as well, proving that every session delivered value and met compliance requirements.
Today’s best practices pair proper documentation habits with smart digital tools, like Raven Health’s AI-powered session note generator, to ensure your documentation stays organized and secure — without eating up your evenings.

ABA Session Note Template Breakdown: How to Structure Your Session Notes
An effective ABA session note template removes guesswork and makes every treatment session crystal clear — for you, your team, and your funding sources.
A strong template ensures you never miss the key session details that demonstrate real client growth and guide your next steps. Each note should paint a clear picture of what happened during ABA therapy, how the client engaged with the session, and what comes next.
Remember, your notes serve as proof of quality care, helping every therapist stay consistent, compliant, and focused on great outcomes.
Key Components of an Effective ABA Note Session Template
| Section | What to Include | Example |
|---|---|---|
| Session Details | Client name, therapist name, session date, location | “July 15, 2025, Center 2” |
| Goals & Targets | Skills or behaviors targeted in this session | “Receptive labeling: 8 new items, increase desirable behaviors during transitions” |
| Specific Behaviors Observed | What you observed during tasks and trials | “Completed 20 trials with prompts faded” |
| Client Responses | Measurable reactions to tasks | “Client independently responded in 75% of trials” |
| Subjective Observations | Non-judgmental context: mood, distractions, environmental notes | “Client was initially distracted by sibling” |
| Objective Data | Percentages, frequencies, durations | “80% mastery across 3 consecutive sessions” |
| Session Summary | What was achieved, what to work on next | “Maintain current targets, add 2 new objects next session” |
| Therapist Signature | Credentials, date | “Signed: Casey Green, RBT” |
Be sure to bookmark this tab, as the table above this provides you with a quick, simple structure for every session. Or better yet, automate it! Raven’s AI-powered session notes tool pulls in key session details automatically, creating a well-aligned, comprehensive notes template that compares each new record to the previous session for easy progress tracking.
With this digital tool, your documentation process stays organized, your team stays informed, and your session notes stay consistent — so you can focus on delivering the best care, not wrestling with paperwork.
ABA Session Notes Examples You Can Use Today
Here’s an example note on how a full ABA session might look after effectively recorded:
Example:
Session Date: July 15, 2025
Objective: Discrete trial training for receptive labeling.
Specific Behaviors Observed: Client participated in 20 trials with 90% accuracy.
Client Responses: Responded independently to 15 trials; required gestural prompts for the rest.
Subjective Observations: Client more engaged after snack break.
Session Summary: Continue current program, introduce 2 new items next week.
Simple, clear, and detailed — that’s what makes effective session notes.
How to Write Effective ABA Session Notes for Any ABA Practice
Want your session notes to work harder for you? Focus on four things:
- Clarity: Be concise, factual, and measurable.
- Consistency: Use the same ABA session note template for every session. This is easy to do, after utilizing a stored program library.
- Compliance: Include every section your funders and insurance providers need.
Be sure to avoid judgmental or opinionated language — stick to observable facts.
This is where many ABA practices get buried in admin. That’s why Raven Health launched the first all-in-one AI ABA notes generator that writes your clinical session notes for you — so your team stays focused on what matters: your clients.
Key Sections Every Notes Template Should Include
Every good ABA session note template includes:
- The session date and location
- Objective: Discrete trial training for receptive labeling.
- The ABA session objectives
- Unique behaviors observed
- Client actions and reactions
- Personal clinical observations
- Measurable data compared to prior sessions
- A short, clear session summary
- Next steps for future sessions
- An ABA therapist’s signature and credentials
Stay consistent and you’ll meet session note requirements every time.
Writing Clear & Measurable ABA Session Notes: Note-Taking Tips
If you’re still writing session notes manually, remember these tried-and-true note-taking habits that keep your documentation strong:
Plutus Health is a dedicated ABA billing company offering comprehensive billing management services. They’re known for helping ABA practices manage intricate billing processes, including coverage validation, authorization management, claim submission, denial follow ups and resolution, and accounts receivable oversight. Plutus Health’s ABA therapy billing experts handle everything from coding compliance to claim rejections, so clinics can maintain focus on patient care instead of paperwork.
- Use clear, measurable data: “Client completed 15 of 20 trials independently.”
- Add personal observations carefully, and always label them so they don’t get confused with measurable facts.
- Stick with third-person writing — avoid “I” or “we” to keep your language professional and consistent with payer requirements.
- Finish session notes promptly after the session ends so you don’t lose details or make mistakes later.
Solid note-taking means more than just meeting compliance standards — it helps you build a full picture of each client’s progress over time. These details will guide you when planning what to target in the next session, and they ensure you have the context you need to adjust strategies or introduce new goals.Many ABA therapists know the frustration of wrapping up a productive ABA therapy block, only to spend an extra hour stuck at a laptop trying to remember exactly how the client responded or which specific behaviors you observed.
That’s why so many clinics are moving to digital platforms that streamline the entire documentation process. Tired of spending hours drafting every detail by hand? Raven Health’s AI-powered solution does the writing for you — instantly generating clear, natural-language session notes that highlight objective data, include key subjective and objective information, and meet strict compliance and payer requirements.
With automated note generation, you’ll finish faster, plan your next session with more confidence, and spend more of your day where it matters most — delivering excellent ABA therapy that changes lives.
Smart ABA Note-Taking for Therapy Sessions: Boost Your Practice
Smart note-taking isn’t just busywork — it’s a powerful way to strengthen your ABA practice and deliver better outcomes for every client you serve.
ABA therapy providers often underestimate the time-consuming admin load that comes with managing billing tasks internally. The truth is, juggling multiple payers, staying updated on insurance services requirements, and managing claim denials can quickly drain your time and resources. That’s why so many practices now rely on trusted RCM services that offer tailored solutions built just for ABA therapy services — covering everything from insurance verification to denial management and accurate reimbursement.When you write ABA session notes effectively, you’re not only capturing what happened in the moment; you’re creating a clear roadmap for the entire care team to follow. Detailed notes help you see patterns over time, so your staff can fine-tune interventions, make data-backed decisions, and celebrate each milestone in your clients’ journeys.
With strong session notes, your team can:
- Spot trends in client progress that might otherwise go unnoticed
- Adjust programs quickly to respond to new needs and goals
- Address unexpected behaviors before they become barriers
- Prevent gaps that lead to claim denials or compliance issues
Today’s best practice management software makes this process even easier. Instead of juggling paper files or scattered documents, your team can log every detail in a secure, centralized system — streamlining everything from daily data entry to insurance submissions. When you pair thoughtful note-taking with smart tools like Raven Health’s AI-driven generator, your clinicians spend less time writing and more time focused on meaningful ABA therapy with clients.

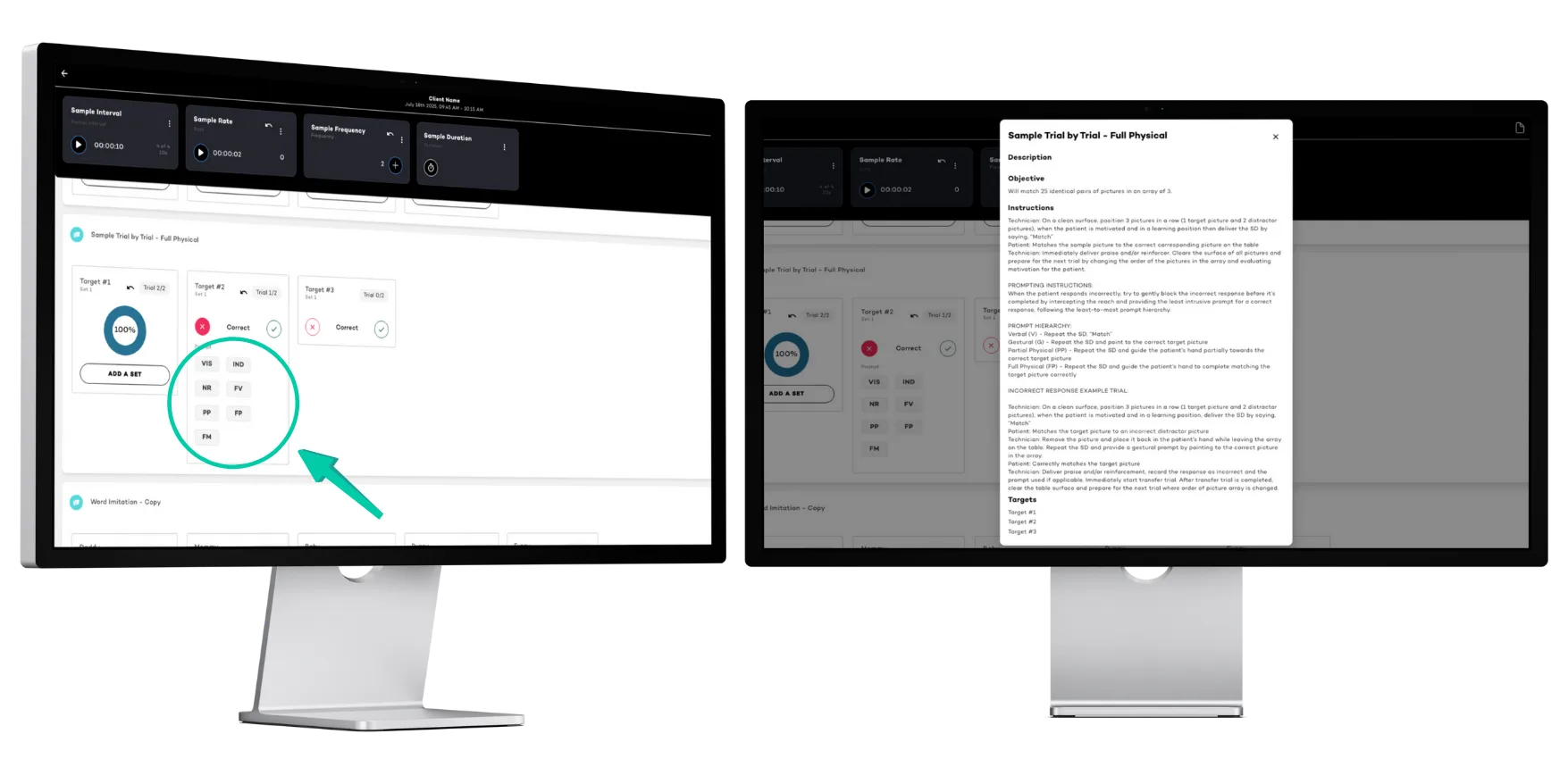
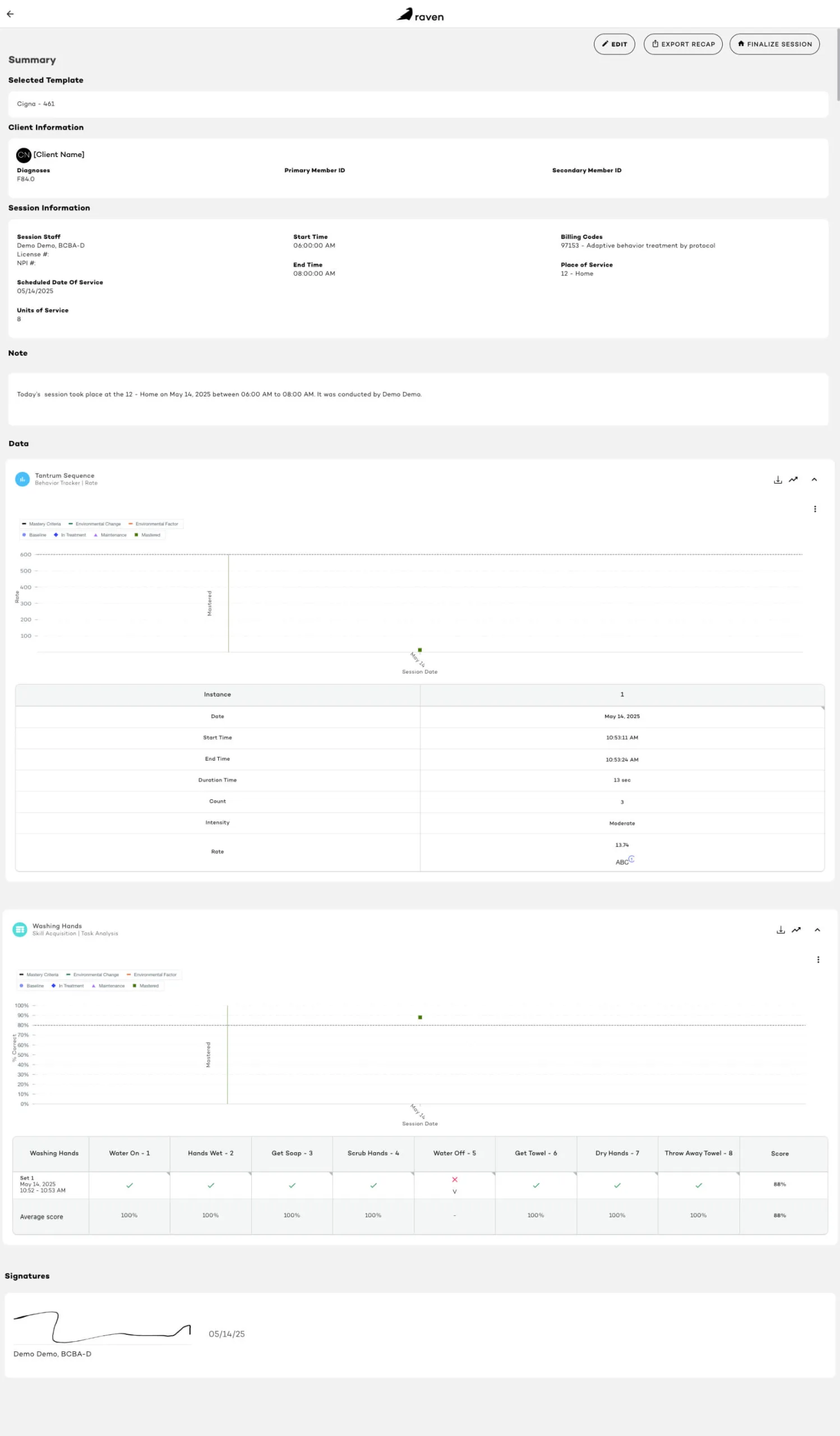
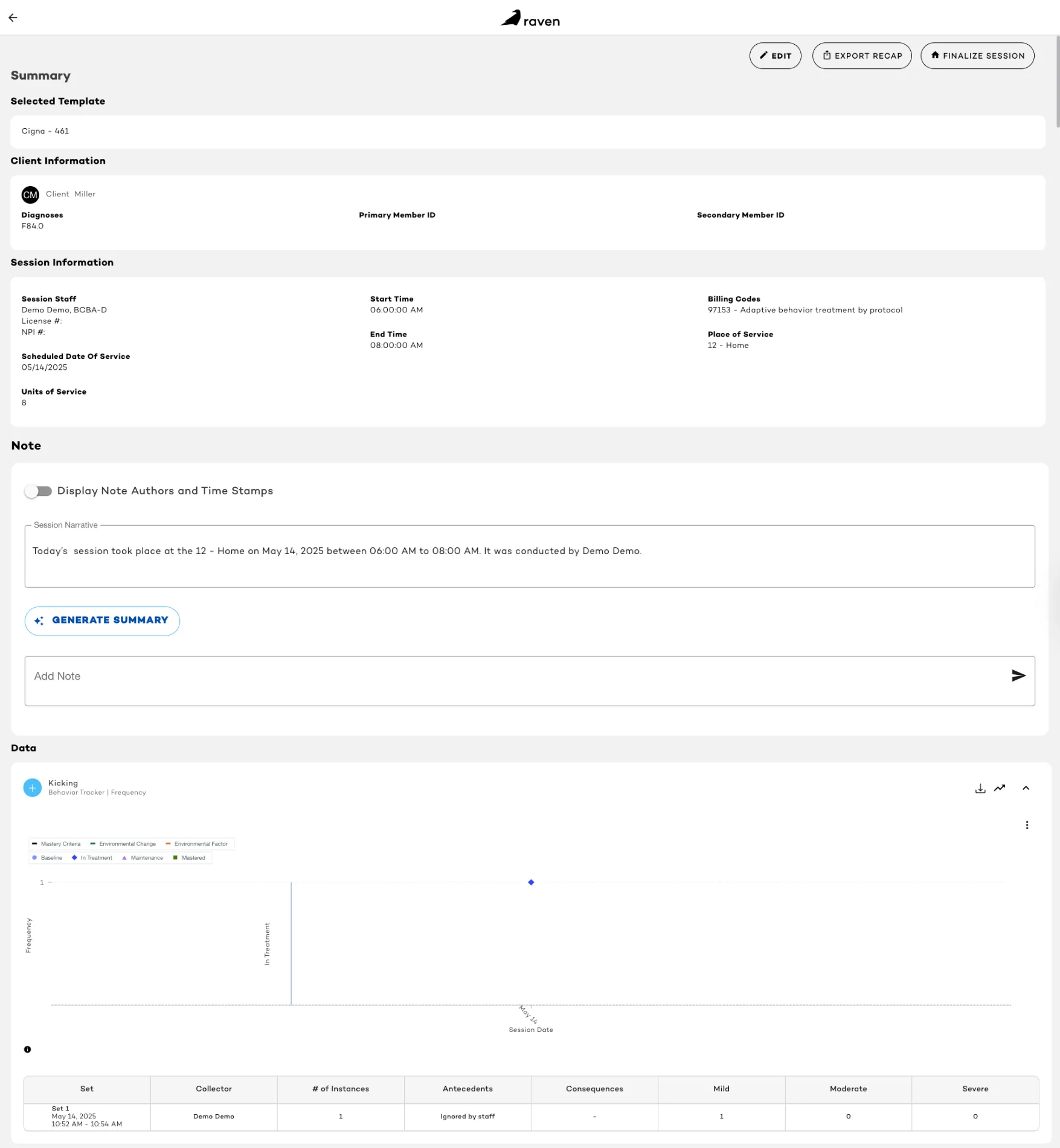
As seen in the rendering above, our AI-backed note-taking process does this automatically, so you and your team can track progress on everything from trial training to token economy systems — all without the stress of manual edits or errors.
Tools & Strategies for Better ABA Session Notes & Note-Taking
Want better session notes? Try this:
- Use one consistent ABA session note template for every treatment session to ensure nothing important is missed.
- Train your team to complete ABA notes promptly after each session, while details are still fresh.
- Highlight clear client progress every time by focusing on key components like goals, targeted behaviors, and measurable outcomes.
- Store your session notes securely in digital form so they’re easy to access, share, and update as needed.
- Let AI generate effective ABA session notes in real time so you can spend more hours with clients instead of typing at your desk.
When you have an organized approach to note-taking, you reduce errors, save time, and protect your practice. A clear, structured process also helps newer team members — like RBTs — feel confident that they’re meeting all session note requirements. Even a simple example note can show your team exactly how to write clear, objective observations and track each client’s progress in a way that’s easy to review later.
With Raven Health’s all-in-one, AI-powered platform, your session notes, billing, scheduling, and clinical documentation all live in one secure system. No more juggling disconnected tools or re-entering the same data multiple times — instead, you can focus on helping clients build new skills, strengthen desirable behaviors, and make meaningful gains that last.
By following these tools and strategies, your practice will be better prepared to deliver high-quality care, demonstrate outcomes for funding partners, and keep your team aligned every step of the way.
👉 Explore Raven’s Complete ABA Practice Management
Using SOAP Note Format for ABA Session Notes
Many BCBAs love the SOAP note format for ABA session notes. SOAP stands for:
- Subjective: Non-measurable context (client seemed tired)
- Objective: Hard data (completed 15 trials)
- Assessment: What it means (client progress on target)
- Plan: What’s next (increase difficulty)
The SOAP notes format holds a simple, proven structure that works well for many ABA therapy sessions
Other Note Template Formats for Applied Behavior Analysis
Besides SOAP notes, you might prefer:
- Checklist style: Quick task checks, great for RBT session notes
- Narrative style: Full paragraphs, great for complex cases
- Hybrid: A blend for busy clinics
Raven Health supports any style — but adds AI to finish the job in seconds, not hours.
Documenting Client Responses in ABA Session Notes
Client responses are the beating heart of good session notes. They show how the client actually performed during each treatment session, so you can confidently plan your future interventions and make meaningful decisions about treatment.
When you document clear, specific responses, you help board certified behavior analysts, supervisors, and ABA therapists understand exactly what happened — what worked well, what needed more support, and how the client’s behavior changed during that session. This level of detail is what turns ordinary notes into effective notes that actually drive results for your clients.
Comprehensive records that include detailed learner responses also strengthen your compliance position with funding sources. Whether you’re sharing updates with families or submitting notes to insurance companies, your documentation proves that services were delivered as planned and that each session contributed to real, measurable growth.
For example:
- “Client responded independently to 80% of prompts.”
- “Client required moderate gestural prompts to complete final tasks.”
- “Client initiated four peer interactions without prompts.”
Good session notes always describe client responses using clear, objective language — not guesswork or vague comments. They capture observable behaviors so your team can track progress session to session and compare outcomes across different goals.
A strong note template makes it easier to keep these details consistent. With a clear template, every provider on your team can follow the same structure, creating comprehensive records that paint a full, accurate picture of each client’s journey.
Ultimately, well-documented client responses help ensure that your session notes are more than just paperwork — they’re a powerful tool that drives your entire treatment plan forward. They keep your whole team informed, demonstrate accountability, and help you deliver the highest standard of care possible.
Subjective Observations vs. Objective Data in ABA Session Notes
Never mix subjective observations with your hard numbers.
- Subjective: “Client appeared restless during DTT.”
- Objective: “Client required 3 prompts to complete the task.”
Good ABA session notes should clearly separate subjective and objective information — subjective details provide context, while objective data proves measurable client progress. Both belong in your ABA session notes, but label them so reviewers — and your team — know which is which.
RBT Session Notes: What Registered Behavior Technicians Must Know
Great RBT session notes follow the same rules as BCBA notes — just focused on implementation, not program design.
Every registered behavior technician should:
✅ Stick to data and client responding to different incentives
✅ Avoid judgmental language
✅ Use your standard ABA session note template
✅ Submit session notes immediately after the therapy session
Raven Health makes this easy — with an AI tool that builds RBT session notes instantly.
RBT Session Notes vs. BCBA Notes: Differences & Best Practices
RBT session notes capture what happened.
BCBA session notes add the clinical “why” and “what’s next.”
One consistent notes template keeps your team aligned — whether you’re logging trial training, token economy system reinforcers, or new goals.
How a Standard ABA Note Template Helps RBT Session Notes
A clear, standard ABA session note template:
✅ Keeps your whole team on the same page
✅ Speeds up the note-taking process
✅ Ensures nothing vital is left out
✅ Protects your clinic from compliance headaches
Combine your notes template with Raven Health’s AI — and you’re unstoppable.
FAQ: Note-Taking, Session Notes & ABA Practice Management
How does practice management software help with ABA session notes?
Practice management software automates your note-taking, organizes client files, and connects clinical documentation with billing workflows so you can get paid faster and reduce administrative burdens. It centralizes scheduling, data collection, and treatment summaries, ensuring nothing slips through the cracks.
What happens if a therapist forgets to write ABA session notes?
Can I use a generic therapy notes template for applied behavior analysis?
Do insurance providers accept handwritten session notes?
How does a strong notes template help team communication?
Consistent session notes strengthen team communication by providing a clear record of what occurred in prior sessions, how the client responded, and what the plan is for future ABA sessions. This transparency ensures that therapists, supervisors, and healthcare providers are all aligned, promoting cohesive and effective client care.
What are the key components that must be included in every session note?
How can I improve the efficiency of my note-taking process?
What is the difference between subjective observations and objective data in session notes?
Can registered behavior technicians (RBTs) write session notes, and how do their notes differ from those of BCBAs?
What role do session notes play in insurance reimbursement?
Are there any compliance risks associated with poor session note-taking?
How do digital tools improve the note-taking process for ABA therapists?
What should I do if I notice inconsistencies or errors in previous session notes?
Can session notes be shared with parents or caregivers?
How often should session notes be reviewed and updated?
Wrapping Things Up: How a Smart Note Template Strengthens Your ABA Practice
At the end of the day, effective ABA session notes aren’t just paperwork — they’re the proof that your therapy is working and your clients are growing. A simple, clear ABA session note template makes your entire ABA practice stronger, more efficient, and far less stressful for everyone involved.
The truth is, even the most skilled therapists can lose valuable hours every week trying to keep up with manual ABA note taking. One late note here, one missed detail there — and suddenly your clinic’s documentation process is behind, insurance claims are delayed, and your team is buried under piles of admin work.
That’s exactly why Raven Health created the first all-in-one AI-powered session notes tool for ABA providers. Unlike other solutions that bolt on expensive add-ons, our AI notes generator comes included — writing your ABA session notes for you, instantly, with accuracy you can trust. Every note is clear, organized, and HIPAA-compliant, so you spend less time worrying about documentation and more time doing what really matters.
When your ABA note taking is smart, automated, and built right into your daily workflow, your entire practice runs smoother. Your team stays aligned, your clients get better results, and your business grows stronger every single session.
Stop spending hours writing session notes by hand — and start spending more time where it counts: face-to-face with your clients, driving real change.
Here are some helpful resources below to aid in additional assistance:
- Learn How to Choose the Best AI ABA Software
- Explore Types of ABA Data Collection Methods
- See Raven’s Complete ABA Practice Management
Ready to Automate ABA Session Notes? See Raven Health in Action
Raven Health empowers BCBAs, RBTs, and clinic owners to generate, store, and share clear, compliant session notes in seconds — no more late nights finishing paperwork by hand. Alongside instant note generation, our intelligent billing engine works behind the scenes to push your reimbursement rates higher, helping small clinics collect nearly 99% of what they’re owed without the headaches of manual claims.
With everything under one roof — scheduling, data collection, AI note taking, and billing — you finally have a smarter, simpler way to manage every session from start to finish. And because we believe in earning your trust, you can test drive our full platform before you commit. Explore how it works at your own pace, then join a live demo to see how other providers are transforming their workflow and freeing up valuable time.
When your notes write themselves, your team gets more hours back to spend with clients and families. When your billing is automated, you keep more of what you’ve earned, with fewer denials and less frustration. And when your tools connect seamlessly, your whole team stays focused on what matters: helping clients achieve meaningful progress, session after session.
If you’re ready to spend less time chasing paperwork and more time making an impact, we’d love to show you how we can help. Schedule a one-on-one walkthrough with our team to see exactly how Raven Health fits your practice — and why so many small providers are switching to an all-in-one solution that actually works.
Take the first step toward more freedom, stronger outcomes, and a practice that runs smarter than ever. book your demo today.