Writing clear and consistent session notes is one of the most important tasks in ABA therapy. Clinicians rely on these notes not only to track a client’s progress but also to meet insurance, ethical, and legal requirements.
One of the most trusted ways to organize those notes is the SOAP format—Subjective, Objective, Assessment, and Plan. This structure helps behavior analysts document what happened in a session in a simple, organized way that anyone on the treatment team can understand.
Whether you’re a new RBT learning to write session notes or a BCBA looking to improve documentation across your team, understanding how the SOAP method works can make your notes clearer and more useful. In this article, you will explore more about SOAP notes and its role in ABA clinics.
What are SOAP Notes, and Why Do They Work for ABA?
SOAP is an acronym that stands for Subjective, Objective, Assessment, and Plan. It was designed to organize clinical thinking and make records easy to read. In ABA therapy, SOAP notes let you capture what caregivers report (Subjective), what you observed and measured (Objective), your clinical interpretation (Assessment), and the next steps (Plan). This structure helps everyone on the team understand a client’s status at a glance.
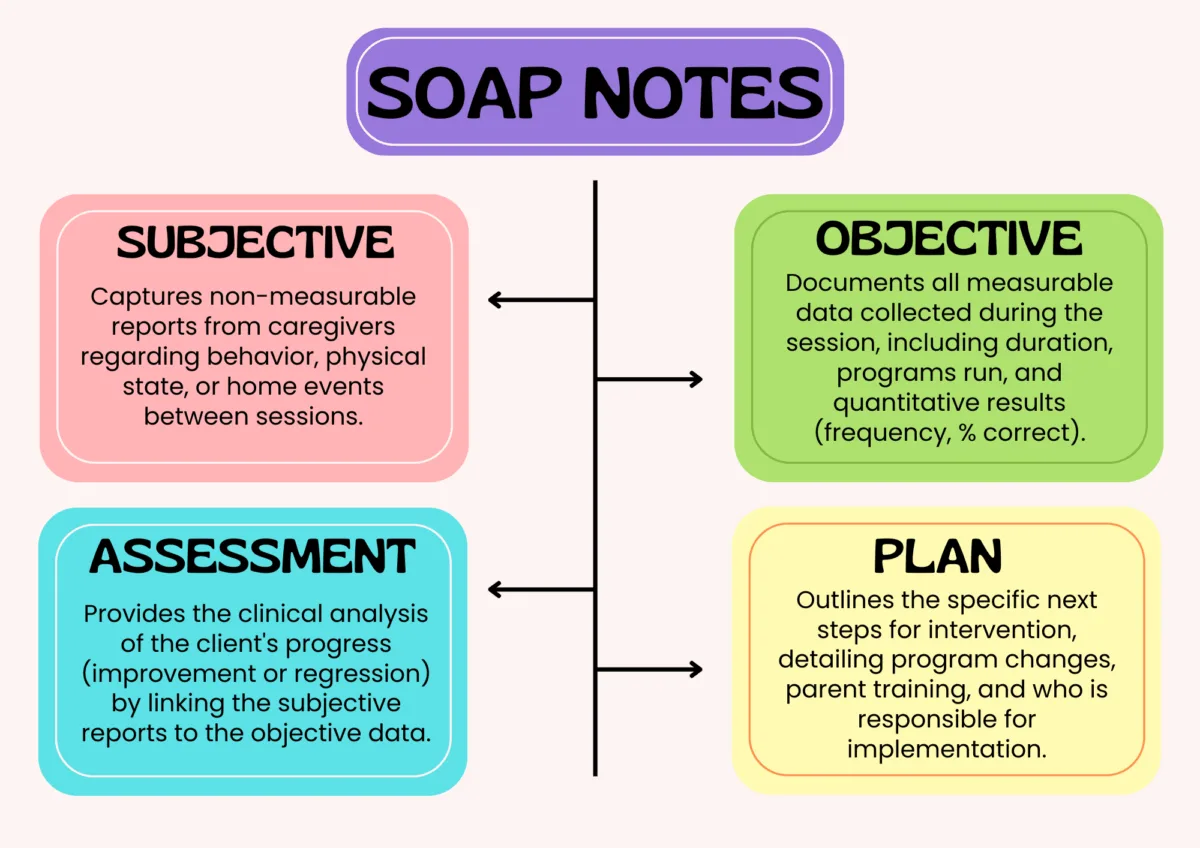
1. Subjective—what caregivers and clients tell you
The Subjective section records reports from parents, teachers, or the client. For ABA this usually includes caregiver feedback about behavior between sessions, family concerns, or home events that might affect therapy (illness, family change, medication changes). Keep it brief and relevant: include the source (who said it), the time frame, and any direct quotes that matter.
2. Objective—what you actually observed and measured
Objective is the most data-driven part for ABA. Enter concrete, measurable information: target behaviors, data (frequency, duration, percentage correct), session length, setting, prompts used, and staff initials. Use consistent units (minutes, counts, percent correct) and reference specific programs or goals by name or ID. These details let supervisors check progress and prepare defensible billing documentation.
3. Assessment—your professional interpretation
In Assessment, you tie the subjective and objective pieces together. Say whether the data shows improvement, plateau, or regression, and explain why in short clinical terms. For example: “The client used independent requests in 70% of opportunities this week, which is an increase from 45% last week. The improvement appears connected to the family using visual cues at home.” This part of the note shows your clinical thinking and how you interpret the client’s progress.
4. Plan—what you will do next
The Plan section lists concrete next steps: changes to prompting, schedules for parent training, recommended reinforcers, or proposed adjustments to programs and goals. Include who will carry out each item (RBT, BCBA, parent), any homework for caregivers, and the timeline for review. Clear plans make follow-up sessions efficient and show intention in the clinical record.
Accuracy and Compliance
SOAP notes force clinicians to separate opinion from fact. The Objective section holds the hard data; Assessment and Subjective give context. Payer auditors and compliance reviewers expect measurable evidence tied to treatment plans; SOAP notes make that link explicit. Keeping concise, data-backed notes reduces denials and strengthens clinical defensibility.
Easier Oversight
Well-written SOAP notes let supervisors scan a caseload quickly. Objective data shows fidelity and progress; assessment flags clinical questions; the plan shows planned changes. This makes spot audits and remote supervision practical and focused. Supervisors can use notes to assign training or to request IOA checks when fidelity looks low.
Billing and Payer Requirements
Insurance payers often require session notes that document medical necessity and progress. SOAP notes that include session duration, billed CPT codes (where applicable), and measurable progress tied to goals make claims easier to defend. Keep copies of authorizations and match billed units to documented session time.
Timeliness, Confidentiality, and HIPAA Considerations
Enter notes promptly, ideally the same day while observations are fresh. Secure notes behind HIPAA-compliant systems and follow your clinic’s access controls. Only include PHI necessary for clinical purposes and avoid unnecessary identifiers in shared summaries. Remember: documentation practices must conform to both ethical codes and privacy law.
Common mistakes to avoid
1. Vague Descriptions
One of the biggest issues in ABA SOAP notes is writing statements like “the client did better today” or “behavior improved.” These phrases don’t tell the reader how the client improved or whether progress is meaningful. Insurance reviewers, supervisors, and other team members need numbers, examples, and clear details.
2. Forgetting Required Administrative Details
It’s easy to focus on the clinical details and forget basics such as the exact start and end time of the session, your full name or initials, or supervisor signatures. However, these details are some of the first things auditors look for. Missing times or signatures can lead to denied claims, compliance concerns, or confusion about who provided the service
3. Mixing Objective Facts with Assessment Interpretations
Another common mistake is combining measurable information (what actually happened) with the clinician’s interpretation of why it happened. In SOAP notes, these belong in two different sections.
- Objective: Data, behavior counts, task analysis results, or direct observations.
- Assessment: Clinical meaning of the data, whether the client is improving, staying the same, or regressing, and why.
When these two pieces are blended, it becomes harder for supervisors or insurance reviewers to understand how the clinician reached their conclusions.
Conclusion
SOAP notes give ABA clinicians a clear, repeatable method to document sessions. When notes are specific, timely, and tied to measurable goals, they improve clinical decision-making, support compliance and billing, and make supervision more effective. Make SOAP part of your practice’s routine: brief, factual entries today save time and reduce questions later.