How to Choose the Best AI ABA Software
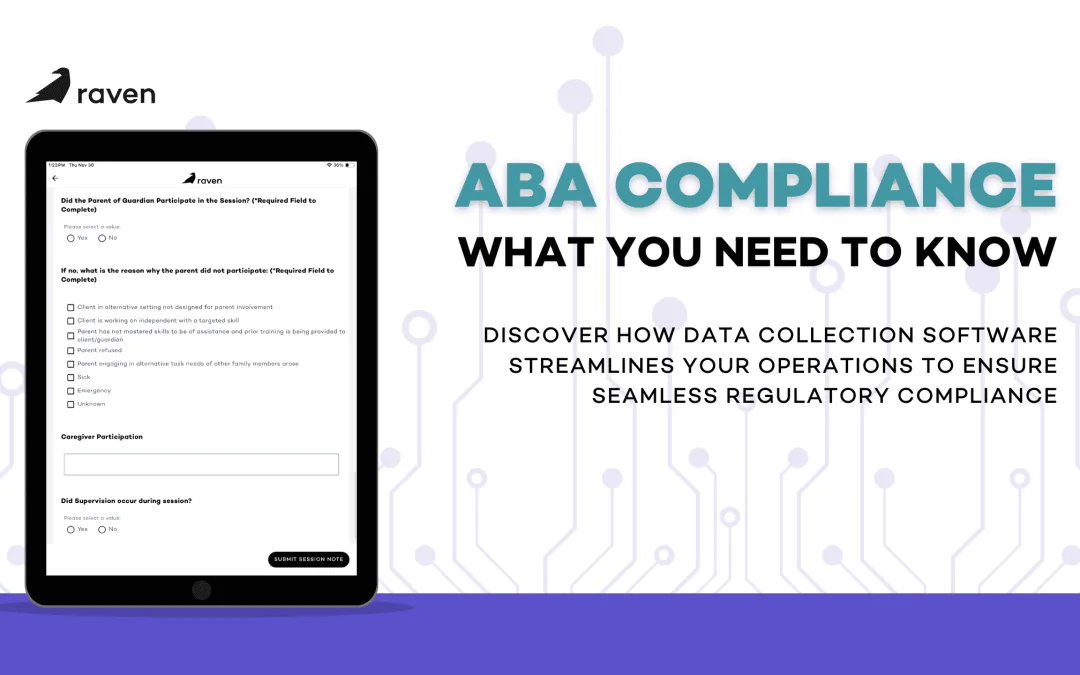
In the evolving world of Applied Behavior Analysis (ABA) therapy, providers are facing more pressure than ever. Clinics are expected to juggle treatment planning, data collection, claims submission, ABA compliance, and team coordination—while still prioritizing outcomes for learners with autism. Sound familiar?
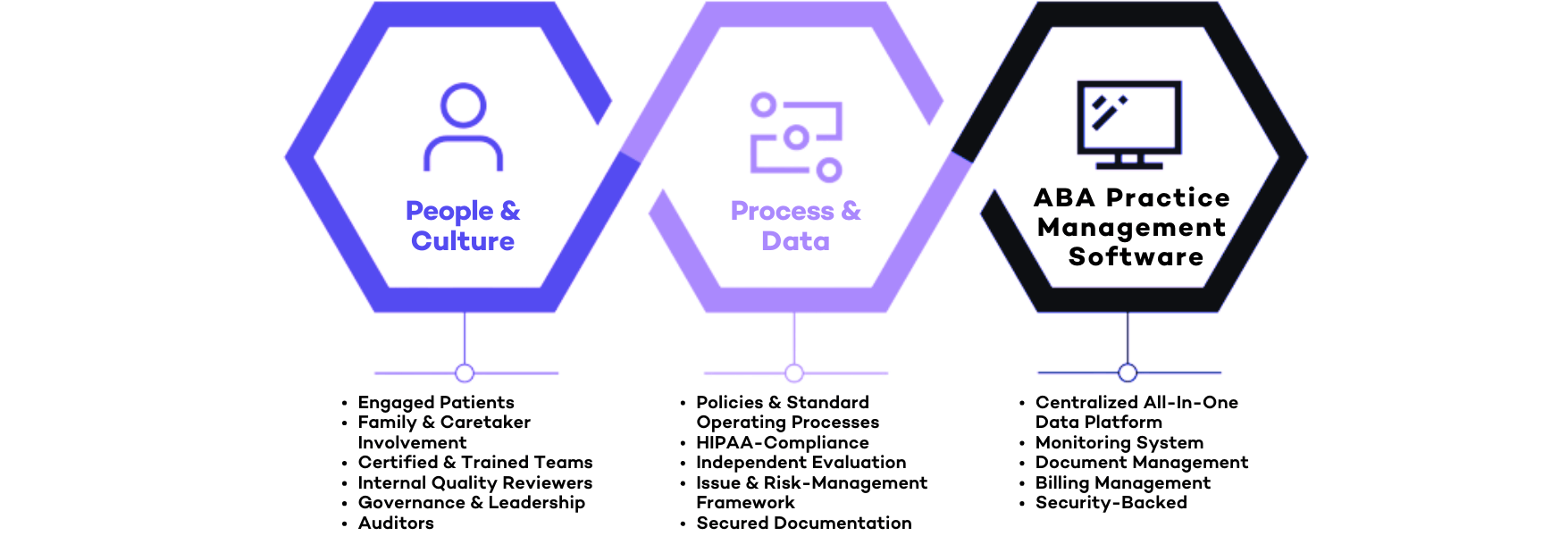
That’s exactly why AI-powered ABA software is no longer a nice-to-have—it’s the backbone of a thriving modern ABA practice. But with a growing number of platforms on the market, finding the right solution for your clinic can be overwhelming. From billing systems and reporting tools to automated session notes and predictive models, it’s essential to choose an all-in-one platform that doesn’t just check the boxes—it transforms your operations and supports scalable, sustainable growth.
Whether you’re a BCBA, RBT, clinic owner, or operations manager, the right AI ABA software should feel like having a second brain behind your practice: working tirelessly to ease day-to-day documentation, handle insurance claims, maintain HIPAA compliance, and unlock better outcomes for your clients. It should simplify the complex, automate the tedious, and empower your staff with the tools they need to deliver exceptional care. In this guide, we’ll break down everything you need to know to choose the most powerful, practical, and future-forward software—and why so many providers are turning to Raven Health’s fully integrated solution to do it all.
What Is ABA Software?
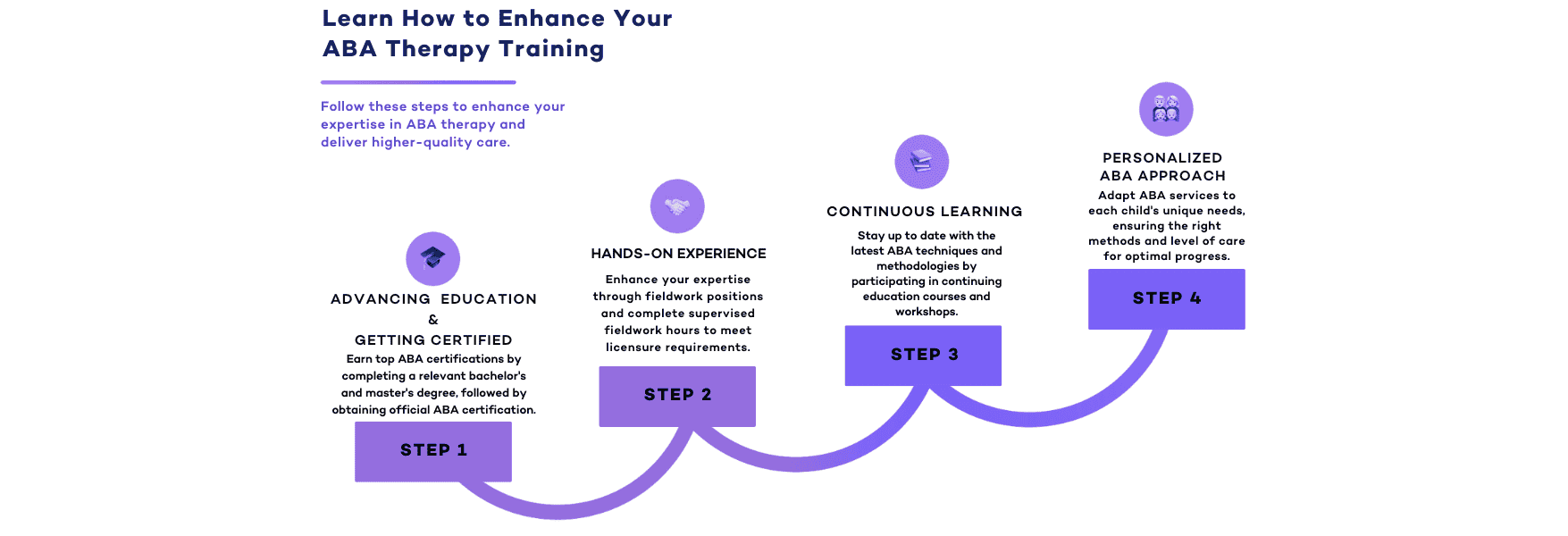
At its core, ABA software is a digital tool that helps behavior analysts and therapy clinics streamline how they run their practice. From session planning and treatment delivery to billing and reporting, it replaces outdated systems and piles of paper documentation with streamlined digital workflows.
But not all software is created equal. Many systems were built before modern challenges emerged—leaving providers stuck with clunky tools, incomplete integrations, and limited support. Today’s top practice management software integrates everything in one place: data collection, session notes, claims, and more.
This type of tool is especially vital for providers serving children with autism, who require individualized care plans and real-time data tracking to make informed decisions. By reducing the hours clinicians take jumping between disconnected systems, advanced software frees up more time to focus on clients and families—not paperwork and processes.
What should you look for? Prioritize tools that offer seamless system integration, intuitive assessment functionality, and strong provider support. Even better, find a platform that anticipates your clinic’s needs by learning from your data, offering insights to improve your day-to-day workflows and clinical outcomes.

Features of AI ABA Software
Not all industry software offers AI capabilities—but the ones that do are setting a new standard for quality and efficiency in therapy delivery. Let’s dive into the most valuable features to look for:
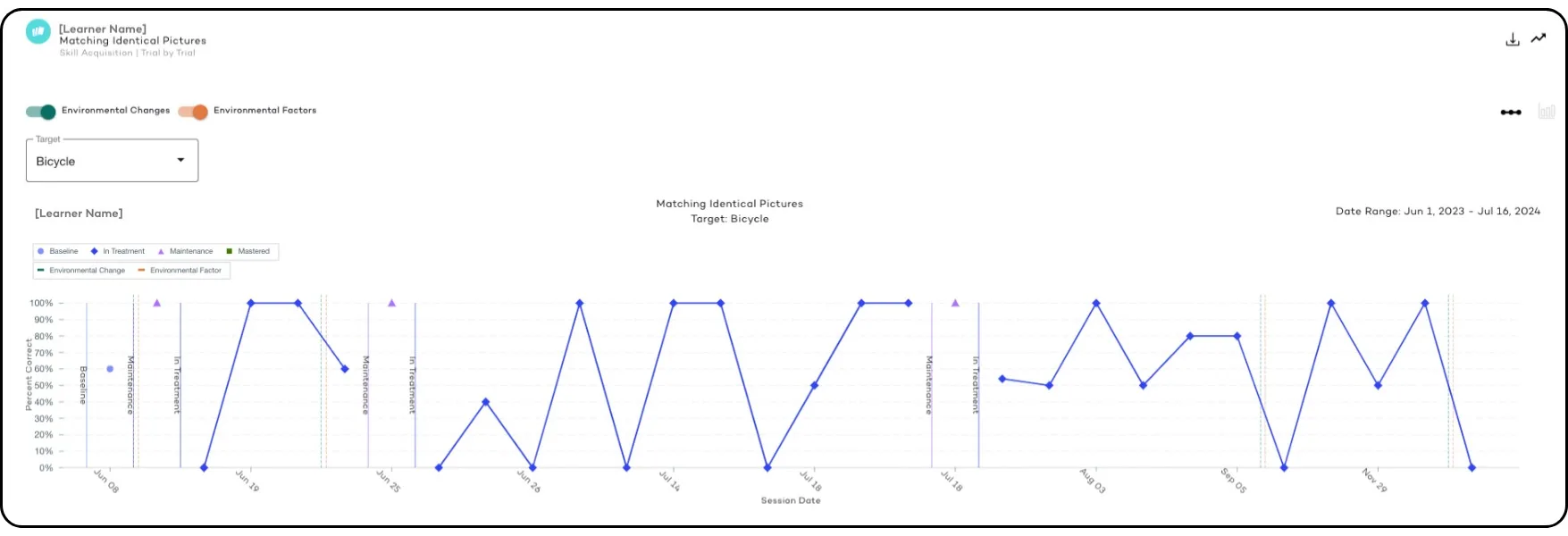
AI-Powered Data Collection and Tracking
Gone are the days of manually recording every behavior. With AI-powered data collection, clinicians can track progress in real-time with fewer clicks. These systems learn from patterns, helping your organization make informed decisions faster. Data becomes more than just numbers—it becomes actionable information that supports better patient treatment and outcomes.
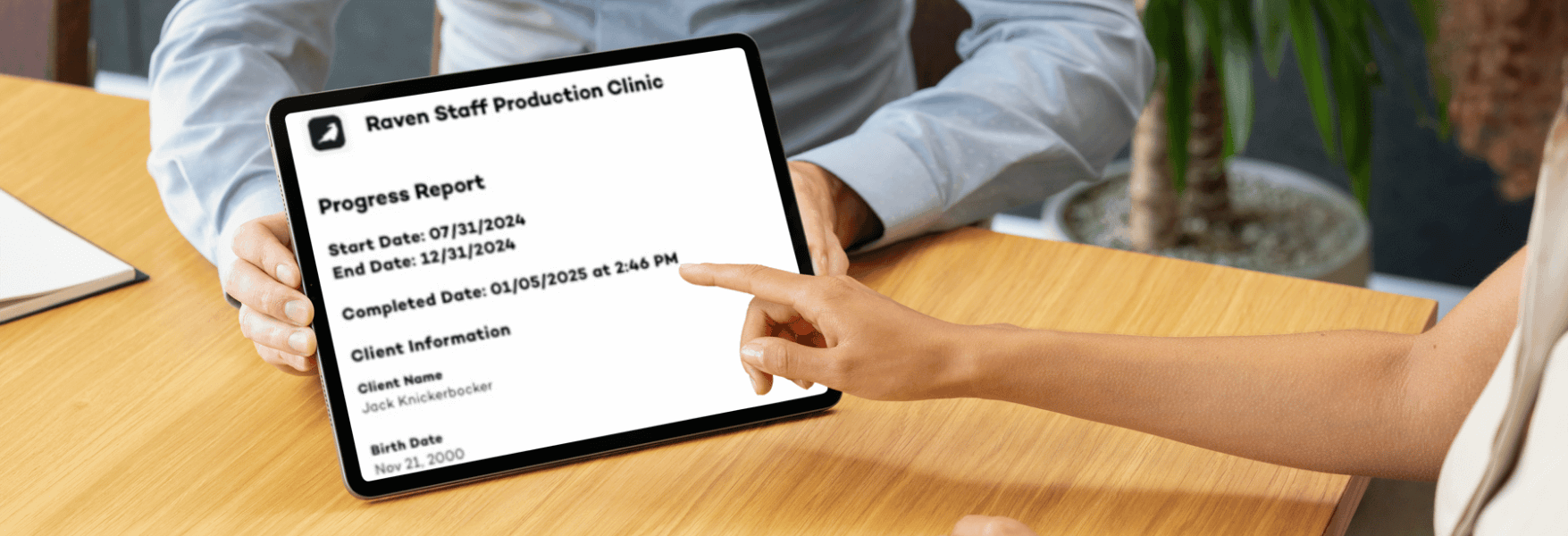
Automated Progress Reports
Say goodbye to spending hours building progress reports. AI systems can auto-generate comprehensive reports that align with insurance requirements, saving valuable time for your clinicians. The result? More consistent documentation and fewer denials when you submit claims.

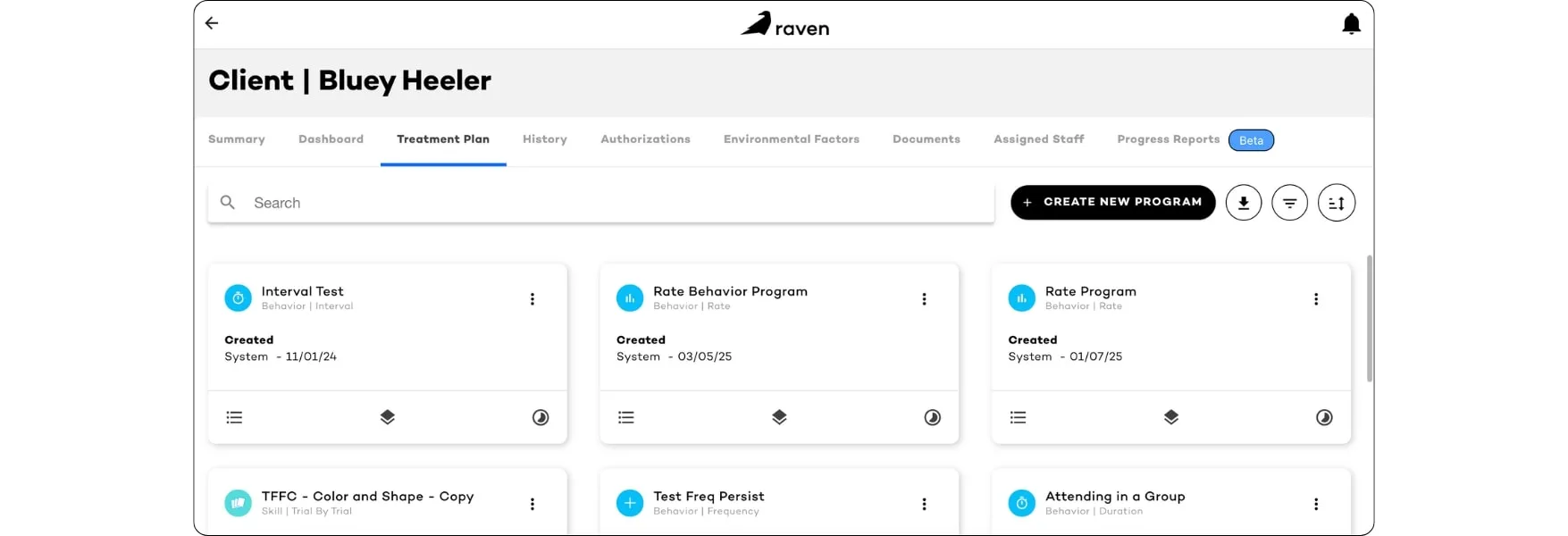
Personalized Treatment Plans
AI models are now smart enough to help build individualized care plans based on real-time assessment data. These dynamic therapy plans evolve with your clients, adjusting based on new insights to provide more precise support.
Behavior Prediction and Analysis
One of the most exciting advances in ABA AI software is predictive analysis. AI tools can detect subtle shifts in behavior patterns, alerting providers before regression occurs. This proactive approach empowers teams to make data-driven decisions, reduce risk, and intervene earlier—ultimately improving patient outcomes.
Benefits of Using AI ABA Software
AI is reshaping every corner of ABA therapy—delivering major value to every stakeholder in the practice. Here’s how:
For Behavior Analysts
AI helps BCBAs spend less time on day-to-day paper documentation and more time focusing on clinical quality. With automated data collection features, treatment notes, and reporting tools, behavior analysts can deliver higher-quality treatment in less time. Plus, Raven Health’s all-in-one software makes it easy to manage assessments, track goals, and access data from a single platform.
For ABA Therapists (RBTs)
Managing a clinic means overseeing people, payments, claims, and backend processes—all while trying to grow. AI-powered industry software like Raven helps streamline everything. From billing automation to denial resolution and HIPAA-compliant documentation, managers gain more control over revenue, resources, and clinic performance.
For Parents
Today’s parents want visibility into their child’s care. AI-powered tools deliver clear, digestible updates on therapy progress, goals, and milestones. It’s not just peace of mind—it’s participation. Families stay informed throughout the treatment, enhancing engagement and transparency.

What to Consider When Choosing ABA AI Software
Every practice is different, so your software should reflect your specific needs. Here’s what to consider when making your choice:
- Clinic Size and Needs
Whether you serve 5 or 50 patients, your software should scale with you. Look for platforms like Raven Health that are built to support small to mid-sized clinics with powerful AI that enhances—not overwhelms—your organization. Your software should grow with your practice, ensuring that as your patient caseload increases, your systems and workflows remain efficient and responsive. - AI Capabilities
Not every platform that mentions “AI” actually delivers. Ask about automated session notes, denial prediction, and adaptive individualized care planning. True AI software should integrate seamlessly into your daily workflows, not sit on the sidelines. Make sure the platform can dynamically respond to changing data and patient behavior, helping clinicians make better decisions and spend more time focused on direct care. - Customization and Usability
Your team shouldn’t need an advanced degree to use your software. Prioritize systems that are intuitive, customizable, and easy to train staff on—without hours of technical setup or steep learning curves. An effective platform should adapt to your workflow, not the other way around. This ease of use also ensures smoother onboarding of new clinicians and consistent patient experiences. - Customer Support and Model Updates
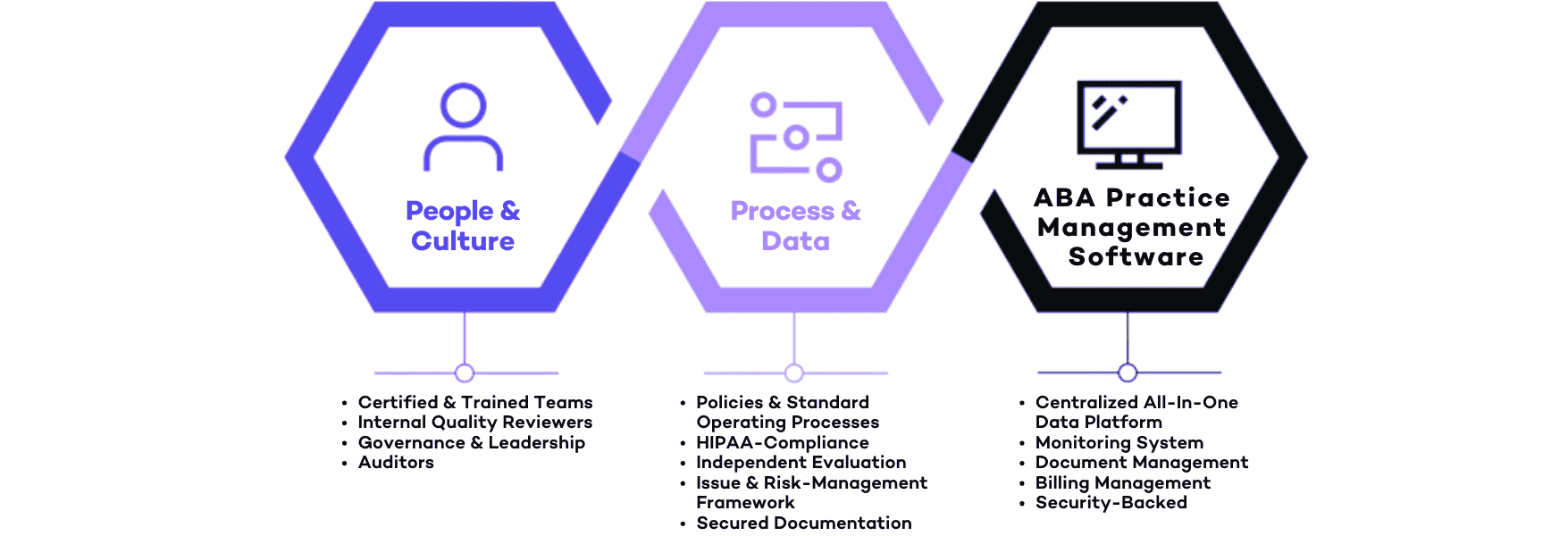
AI evolves constantly. Look for a provider that updates its AI enhancements regularly and offers dedicated support and training to keep your clinicians on the cutting edge. Support should go beyond technical troubleshooting—it should include guidance on how to best use AI to improve results for your patients and streamline your clinic’s operations. - Compliance and Security
Always choose software that’s HIPAA compliant and prioritizes patient privacy. With Raven Health, security isn’t just a feature—it’s foundational. Your patients’ data must be protected with end-to-end encryption, routine audits, and built-in safeguards that ensure full compliance at every level of care. - Integrated Services and Accessible Resources
Finally, consider how well the software integrates with your existing systems and offers value beyond documentation. The best platforms centralize your resources and services—such as scheduling, billing, and clinical documentation—in one unified hub. Easy access to everything your staff needs increases efficiency and helps you stay patient-focused. By combining essential services under one roof, you reduce administrative burden and free up more time for what really matters: delivering the best care to your patients.

How Much Does AI ABA Software Cost?
Pricing for AI-driven software varies depending on the size of your practice and the features you need. While some platforms charge separately for billing, data collection, and session notes, others combine everything into a single package.
Many legacy systems come with expensive upfront costs or rigid subscription models—making it tough for smaller clinics to justify the spend. In contrast, Raven Health’s all-in-one pricing is designed with flexibility in mind. We offer transparent, performance-based pricing that ensures you only pay when you get paid.
This model helps clinics of all sizes—including new or expanding providers—access advanced tools without overextending their budgets. With more accessible pricing, your team can confidently adopt high-quality technology that supports better results for individuals with autism, without sacrificing financial sustainability.
Whether you’re running a solo practice or managing a growing organization, it’s important to choose a platform that grows with you and your clients. With Raven Health, you don’t have to compromise on features or affordability.
Want to see how Raven compares to other options? Check out our pricing page here.
Wrapping Up: Power Your ABA Practice with AI
The future of ABA therapy is smarter, faster, and more connected—and the right AI ABA software helps you achieve it. With features like AI-powered session notes, HIPAA-compliant claims processing, and real-time insights, today’s tools can transform how you deliver services.
For small to mid-sized ABA providers, Raven Health is more than just a software—we’re a partner. Our single platform combines AI billing, documentation, reporting, and scheduling in one seamless solution, so your clinicians can focus on what matters: clients, results, and impact.
Plus, with AI-powered compliance tools, you’ll stay ahead of regulatory requirements without added risk or overhead. Stay on top of trends shaping the ABA landscape, and position your practice for lasting success.
Raven Health doesn’t just streamline operations—it empowers your entire team. Gain access to predictive analytics, personalized treatment insights, and tools designed to scale with your growth. Whether you’re managing a new clinic or an expanding team, you need a smart, flexible platform that keeps up with your pace and priorities.
Whether you’re starting fresh or upgrading outdated systems, now is the time to adopt the right technology for your ABA team. Spend less time on paperwork. Reduce claim denials. Achieve better outcomes. And unlock the full potential of your clinic—with Raven Health leading the way.
Ready to see what AI-powered ABA software can do for you? Book a demo with Raven Health today, or jump right in with a risk-free 30-day trial. We’re here to help—because every minute saved is a minute back with your learners!